What is Macular Hole?
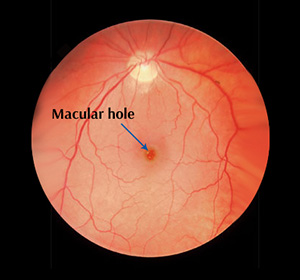
A macular hole is a defect in the macula, the central part of the retina (light receptive tissue of the eye).
The macula is responsible for the sharp central vision required for reading, driving, etc. The central part of the macula called the fovea provides the best possible sharpest vision and is the part of the eye affected by macular holes.
In the early stages, a macular hole causes distorted or blurred vision and straight lines may appear bent or wavy. You may have difficulty with reading and other work that requires seeing detail. As the condition progresses, you can see a blind spot (small dark spot) in the centre of the visual field.
Macular holes are more common in women than men and usually occur in people over 50 years old due to anatomical changes that occur in the eyes with ageing.
The vitreous, a gel-like substance that fills the centre of the eye, is firmly attached to the retina, but with ageing, the vitreous gel shrinks and pulls away from the retina causing a macular hole.
Other factors that can cause a macular hole include severe near-sightedness, blunt injury to the eye, severe swelling of the retina or its detachment from the underlying layers of tissue.
Three stages to a macular hole based on its size and progression
- Stage 1 (foveal detachments) – If left untreated, about 50% of stage 1 macular holes will progress.
- Stage 2 (partial-thickness holes) – If left untreated, 70 per cent of holes will progress.
- Stage 3 (full-thickness holes) – affect central and detailed vision. If left untreated, a stage 3 macular hole can lead to detachment of the retina from the underlying layers of tissue.
Diagnosis of Macular Hole
To diagnose a macular hole, the doctor will instil eye drops and dilate your pupils to view the retina. A test called fluorescein angiography is performed that uses a special dye to illuminate areas of the retina.
Another accurate diagnostic test is the optical coherence tomography (OCT) which uses a laser camera to capture pictures of the retina in which small macular holes that cannot be identified in a Fluorescein angiography can be detected.
If the macular hole is very small and does not cause a major impact on vision, treatment may not be required, but regular eye examinations are recommended to ensure the macular hole does not enlarge or have other effects on the eye.
However, in many cases, surgery is required to improve vision. Vitrectomy is the most effective surgery for a macular hole.
Treatment
I usually treat macular holes with an operation known as a Vitrectomy. I can combine this with Cataract Surgery.
During vitrectomy, I insert very fine instruments through the white of your eye, into the back of the eye and I slowly cut and suck away the vitreous jelly.
In most cases of macular hole, the inner lining of the retina known as the Internal Limiting Membrane (ILM) can be quite stiff and splint the hole open. For this reason, I remove the ILM during the surgery.
After the vitreous and ILM are removed, I search the retina for any other problems and I can treat those too. Once this is all done, I replace the vitreous jelly with a gas bubble. This bubble helps the macular hole to close up.
After the operation, I may ask you to position your head looking down towards the floor (posturing) for 3 days after the surgery. This often helps bigger holes to close. Smaller holes, often close without posturing, so I do not ask all patients to posture. I will discuss this with you in detail, depending on your eye.
Outcomes of Macular Hole Surgery
Overall, about 9 out of 10 of macular holes will close with one operation, so it is unusual to have to repeat surgery. My macular hole closure rate is in excess of 95%.
In nearly all patientshaving macular hole surgery, vision will be stabilised and any further loss of vision is prevented, so surgery is worthwhile.
Approximately 7 out of 10 patients will have at least 2 lines of vision improvement on the vision test charts.