Introduction
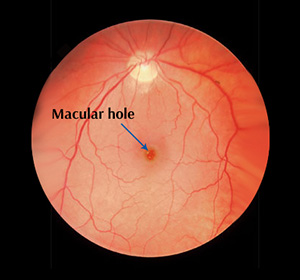
A macular hole is a small break in the macula, the central part of the retina responsible for sharp, detailed vision needed for activities such as reading and driving. The central-most area of the macula, called the fovea, is essential for the clearest vision and is directly affected by this condition. Macular holes often develop gradually, starting with blurred or distorted vision, and may progress to a dark or blank spot in the centre of sight. They most commonly occur in people over the age of 50, often due to age-related changes in the eye’s vitreous gel, but can also result from injury, severe short-sightedness, or other retinal conditions. Prompt diagnosis and appropriate treatment are key to preserving vision and preventing further visual loss.
Causes and Risk Factors of Macular Hole
What Causes a Macular Hole?
A macular hole develops when the delicate tissue at the centre of the retina (the macula) becomes stretched or pulled apart, creating a small break that disrupts central vision. This often happens due to natural changes in the eye’s vitreous gel as we age, but it can also be triggered by other eye conditions or trauma. Knowing the causes and risk factors is important for early diagnosis and treatment.
Common causes and risk factors include:
- Ageing – Most cases occur in people over 50 due to shrinkage and separation of the vitreous gel from the retina.
- Gender – Women are more frequently affected than men.
- High Myopia (Severe Short-Sightedness) – Increases the likelihood of retinal stretching and hole formation.
- Eye Injury or Trauma – Direct impact to the eye can damage the macula.
- Retinal Conditions – Severe swelling of the retina (macular oedema) or retinal detachment can lead to macular holes.
- Vitreomacular Traction – When the vitreous gel pulls abnormally on the macula instead of separating cleanly.
- Previous Eye Surgery – Certain procedures may slightly increase the risk, particularly if the retina is already fragile.
Awareness of these factors highlights the importance of routine eye examinations, especially for those at higher risk, to protect central vision and catch early changes before they progress.
Types of Macular Hole
The Different Stages of a Macular Hole
Macular holes are classified into stages based on their size, depth, and how much they disrupt central vision. Identifying the stage is essential for determining the best treatment approach and predicting visual outcomes.
Stage 1 – Foveal Detachment
Description:
Early stage where the central part of the macula (fovea) begins to lift or detach, but a full hole has not yet formed.Who it affects:
Often detected in patients over 50 during routine eye exams, sometimes before noticeable vision loss.Speed of progression:
Around 50% progress to later stages if untreated.
Stage 2 – Partial-Thickness Macular Hole
- Description:
The hole has started to form but does not extend through the full thickness of the retina. Central vision is usually affected, with distortion or blurring becoming more noticeable. - Who it affects:
Patients whose Stage 1 hole has progressed, or those with vitreomacular traction from age-related changes. - Speed of progression:
About 70% advance to full-thickness holes without intervention.
Stage 3 – Full-Thickness Macular Hole
Description:
The hole extends through the entire thickness of the retina at the macula, causing a central blind spot and significant distortion of straight lines.Who it affects:
Typically individuals whose partial-thickness hole has progressed; may also occur following trauma or retinal detachment.Speed of progression:
Often develops within weeks to months; without treatment, vision loss can be permanent and may lead to further complications such as retinal detachment.
Each stage requires tailored management, from close monitoring in early stages to surgical repair for advanced holes, with the aim of preserving and restoring central vision.
Early Signs & Symptoms
Common Symptoms of a Macular Hole
Recognising the early signs of a macular hole is essential for preserving central vision and preventing further deterioration. Symptoms often begin subtly but can progress quickly, making regular eye examinations important for at-risk individuals.
- Blurred or distorted central vision – Straight lines may appear bent, wavy, or blurred, especially when reading or focusing on detail.
- Small dark or blank spot in the centre of vision – As the hole progresses, a central blind spot may appear.
- Difficulty with detailed tasks – Fine activities such as reading small print, sewing, or recognising faces become harder.
- Reduced clarity in one eye – Vision loss typically affects one eye at first, making it less obvious until tested.
- Changes in contrast and colour perception – Colours may seem duller or less vibrant when viewed with the affected eye.
Early diagnosis offers the best chance for successful treatment and visual recovery, especially if surgical repair is performed before significant vision loss occurs.
Diagnosis and Treatment of a Macular Hole
A macular hole is diagnosed through a comprehensive eye examination, often starting with dilated fundoscopy to closely inspect the retina. Advanced imaging, particularly optical coherence tomography (OCT), provides detailed cross-sectional images of the macula, allowing detection of even very small holes and assessment of their stage. In rare cases, fluorescein angiography may be used to rule out other retinal conditions.
Treatment depends on the hole’s size, stage, and effect on vision. Very small or early-stage holes may be monitored with regular check-ups. However, most macular holes require surgical repair to improve vision and prevent further loss. The standard procedure is a vitrectomy, in which the vitreous gel is removed and replaced with a gas bubble to help the hole close. In some cases, cataract surgery may be performed at the same time. Early surgical intervention offers the highest chance of visual recovery and long-term stability.
Why Timely Diagnosis Matters
Early diagnosis of a macular hole is crucial to preserve central vision and maximise the chances of a successful surgical outcome. If left untreated, a macular hole can progress to advanced stages, causing permanent central vision loss and, in rare cases, retinal detachment. Detecting the condition early allows for prompt treatment before significant damage occurs.
Timely diagnosis enables your ophthalmologist to:
- Identify small or early-stage holes before major vision loss occurs
- Monitor changes in the macula and decide the best timing for intervention
- Prevent further enlargement of the hole through early surgical repair
- Maximise the likelihood of visual recovery after surgery
- Educate patients on recognising symptoms and the importance of follow-up care
Catching a macular hole early can mean the difference between preserving clear, central vision and facing irreversible loss.
Continue Learning About Other Eye Conditions
Other Eye Conditions
The eyes are the most complex sensory organ in our bodies. The eyes provide vision by recording images of our surroundings that the brain will interpret. Although the eye measures only about an inch...
Retinal Vein Occlusion
The retina is the light-sensitive layer present at the back of the eye. It contains nerve cells that convert the focused image to an electrical signal which is then transmitted to the brain.
Worried About Your Vision?
Schedule a consultation with Mr. Mo Majid to evaluate your eye health.
Quick Answers About Macular Hole
What causes a macular hole?
It is usually caused by age-related changes where the vitreous gel shrinks and pulls on the macula, creating a small tear or hole. Other causes include eye injury, severe short-sightedness, or retinal swelling.
Can a macular hole cause sudden vision loss?
Vision loss from a macular hole typically develops gradually, starting with distortion or blurring, but it can worsen over weeks to months if untreated.
Is surgery the only treatment for a macular hole?
Surgery (vitrectomy) is the most effective treatment for most macular holes, especially if vision is significantly affected. Very small holes with minimal symptoms may sometimes be monitored without immediate surgery.