Introduction
What Is Diabetic Retinopathy?
Diabetic retinopathy is a progressive eye condition caused by damage to the tiny blood vessels in the retina due to consistently high blood sugar levels. It’s one of the most common complications of diabetes and a leading cause of preventable blindness in working-age adults worldwide.
The condition often develops without early symptoms, making regular eye exams crucial for people with diabetes. If left untreated, diabetic retinopathy can progress from mild changes to severe vision loss. However, with early detection, good blood sugar control, and timely treatment, most people can preserve their sight and manage the condition effectively.
Causes and Risk Factors of Diabetic Retinopathy
What Causes Diabetic Retinopathy?
Diabetic retinopathy is caused by prolonged high blood sugar levels damaging the small blood vessels in the retina — the light-sensitive tissue at the back of the eye. Over time, these blood vessels can leak, swell, or close off entirely, reducing oxygen supply to the retina and leading to vision problems or even blindness if left untreated.
Key risk factors include:
- Type 1 or Type 2 Diabetes – The longer you have diabetes, the higher the risk of developing retinopathy
- Poor blood sugar control – Consistently high blood glucose accelerates retinal damage
- High blood pressure – Increases the stress on already weakened blood vessels
- High cholesterol levels – Can worsen blood vessel damage and increase risk of leakage
- Pregnancy – Can temporarily worsen diabetic retinopathy, particularly in women with existing diabetes
- Kidney disease – Often linked with diabetic complications that affect the eyes
- Smoking – Contributes to vascular damage and increases overall risk
- Lack of regular eye exams – Early stages may show no symptoms, so undiagnosed progression can occur
Managing blood sugar, blood pressure, and cholesterol — alongside regular eye checks — are critical steps in reducing the risk and severity of diabetic retinopathy.
Types of Diabetic Retinopathy
The Different Types of Diabetic Retinopathy
Diabetic retinopathy progresses through several stages, each with different risks and levels of vision threat. Identifying the stage helps determine the urgency and type of treatment needed.
Background Diabetic Retinopathy (BDR)
Description:
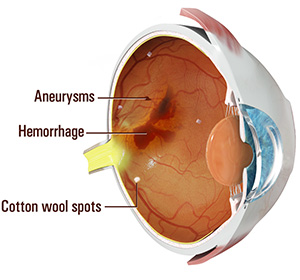
The earliest stage of diabetic retinopathy. It involves small changes in the retinal blood vessels, including microaneurysms, dot and blot haemorrhages, and fluid leakage. Often asymptomatic at this stage.Who it affects:
Common in both Type 1 and Type 2 diabetics. In Type 2, it may already be present at diagnosis.Speed of progression:
Usually slow. May remain stable for years, but regular monitoring is essential to detect changes.
Pre-Proliferative Diabetic Retinopathy
- Description:
A more advanced stage of BDR, showing increased retinal abnormalities such as venous beading, larger haemorrhages, and cotton wool spots. Indicates worsening retinal oxygen supply. - Who it affects:
Diabetics with longstanding or poorly controlled blood sugar levels. - Speed of progression:
Moderate. Some patients may progress to proliferative stage within months if left untreated.
Proliferative Diabetic Retinopathy (PDR)
Description:
The most severe form, marked by abnormal new blood vessel growth (neovascularisation) due to retinal ischemia. These vessels can bleed into the eye and cause complications like retinal detachment.Who it affects:
Typically affects patients with uncontrolled or long-standing diabetes.Speed of progression:
Fast. Without treatment, PDR can lead to sudden and permanent vision loss.
Clinically Significant Macular Oedema (CSME)
Description:
Swelling in the macula caused by fluid leakage from damaged capillaries. It can cause blurred or distorted central vision, even when other parts of the retina are unaffected.Who it affects:
Can occur at any stage of diabetic retinopathy, but more common in advanced stages.Speed of progression:
Variable. May worsen gradually or flare quickly, requiring prompt treatment.
Early Signs & Symptoms
Common Symptoms of Diabetic Retinopathy
Recognising early symptoms of diabetic retinopathy is key to preventing vision loss. In many cases, damage may already be present before symptoms become noticeable — which is why regular eye exams are so important.
- Blurred or fluctuating vision
Vision may become unstable, with sharpness changing from day to day. - Dark spots or floaters
You may see floating spots, cobwebs, or dark strings in your field of vision. - Difficulty seeing at night
Night vision can gradually deteriorate, making low-light environments harder to navigate. - Colours appear faded or washed out
A decrease in colour intensity or contrast may occur. - Empty or dark areas in your vision
These can develop in the central or peripheral field of view as the disease progresses. - Sudden vision loss
Advanced stages may cause rapid, painless vision loss due to bleeding or retinal detachment. - Visual distortions
Straight lines may appear wavy, or you might struggle with depth perception.
Diagnosis and Treatment of Diabetic Retinopathy
Diabetic retinopathy is diagnosed through a comprehensive dilated eye examination. Your eye doctor will use special eye drops to widen the pupils, allowing clear visualisation of the retina. Using a slit lamp and ophthalmoscope, they assess for signs such as haemorrhages, microaneurysms, or abnormal blood vessels. Additional imaging tests — like fluorescein angiography or optical coherence tomography (OCT) — may be used to detect fluid leakage or retinal swelling.
Treatment depends on the severity and type of diabetic retinopathy. In early stages, regular monitoring and tight blood sugar control may be all that’s needed. For more advanced cases, options include focal or scatter laser photocoagulation, intravitreal anti-VEGF injections, or vitrectomy surgery to address bleeding, macular oedema, or retinal detachment. Prompt diagnosis and timely treatment are essential to prevent permanent vision loss.
Why Timely Diagnosis Matters
Diabetic retinopathy is a progressive condition that can silently damage the retina over time, often without noticeable symptoms until vision is significantly affected. Early diagnosis is crucial to prevent irreversible damage and vision loss. Timely treatment can slow or halt disease progression, preserving eyesight and reducing the risk of serious complications such as retinal detachment or blindness.
Key reasons to prioritise early diagnosis:
- Diabetic retinopathy can worsen without symptoms
- Early treatment reduces risk of severe vision loss
- Prevents development of complications like macular oedema and neovascularisation
- Timely care improves treatment effectiveness and outcomes
- Regular monitoring helps maintain long-term eye health
Continue Learning About Other Eye Conditions
Other Eye Conditions
The eyes are the most complex sensory organ in our bodies. The eyes provide vision by recording images of our surroundings that the brain will interpret. Although the eye measures only about an inch...
Vitreous Haemorrhage
Vitreous/vitreous humour, mainly composed of water, is a clear gel-like substance located between the crystalline lens and the retina (light receptive tissue) inside the eye.. It fills the centre of the eye...
Worried About Your Vision?
Schedule a consultation with Mr. Mo Majid to evaluate your eye health.
Quick Answers About Diabetic Retinopathy
How can I reduce my risk of diabetic retinopathy?
Maintaining good control of your blood sugar, blood pressure, and cholesterol levels, along with regular eye check-ups, are key to lowering your risk.
Does diabetic retinopathy affect both eyes?
It usually impacts both eyes, but symptoms and severity can differ, so both eyes should be monitored carefully.
What tests are used to diagnose diabetic retinopathy?
Doctors use a dilated eye exam to look for retinal changes, often supported by imaging tests like OCT scans or fluorescein angiography for a detailed view.